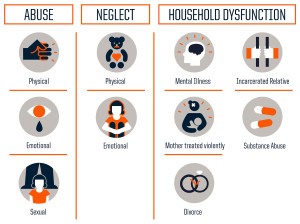
Three types of adversity that make for a tough childhood.
*CRS Q/A Question: What are your thoughts and experience with screening for adverse childhood experiences (ACES) and use of trauma-informed care as one way to improve diabetes outcomes (our experience suggests that ACES are different from PHQ depression and diabetes distress)?
Wow. Great question. Although I am not an expert in this area, I know that ACES are becoming more and more of a focus in the care of children – and rightly so. Kids who have experienced trauma respond in a variety of ways and it makes sense for health care professionals to know how to effectively approach and work with them.
I have heard horror stories about people who’ve been turned away from diabetes providers because they haven’t been seen in over a year. This makes absolutely no sense. If someone is making the effort to be seen, after a long time away is precisely when they need an appointment the most! Not being seen for an extended period of time could be an indicator of a traumatic event in their life. As diabetes professionals, we can be aware of small clues like this and make people feel welcome.
The strengths-based approach encourages us to identify what people are doing well – or at all – and focusing on that. We can even apply those strengths to other areas that need work or improvement. This could be an effective way to work with those with ACES.
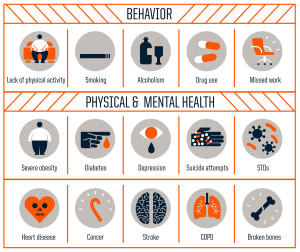
According to the Adverse Childhood Experiences — ACE — study, the rougher your childhood, the higher your score is likely to be and the higher your risk for various health problems later.
All people need hope in their lives. I can only imagine how badly people who’ve experienced trauma need hope. The way we interact with and speak to those with ACES can make a big difference. As always, awareness is the first step.
Images Credit: Robert Wood Johnson Foundation; Source: CDC.
