A situation I experienced tonight made me decide to post the following:
If you take mealtime insulin, avoid taking it too far ahead of a meal. This type of insulin is meant to “cover” or compensate for the meal you are about to eat. Because it works fast, if you take it too soon, there is a risk of going low (hypoglycemia).
Humalog, Novolog, and Apidra (usually called “rapid-acting”) start working in approximately 10 minutes and their peak action happens in about 90 minutes. Within just a few hours, they are gone (although how long they last can vary from person to person). So if you are at home preparing your own meal, it makes sense to take it shortly before you start eating. That way, the insulin has a chance to get started and is working when the food you eat turns to glucose in your blood stream.
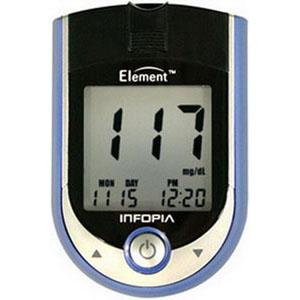
I try to take my rapid-acting (mealtime) insulin about ten to fifteen minutes before I start eating. If my blood glucose is low prior to a meal, I take my insulin and eat immediately – or even treat the low by eating some sort of carbohydrate food first and then take the insulin. If my blood glucose is high, I take my insulin about 20 minutes before I start eating. This way it really has a chance to get to work lowering my blood glucose before I go and raise it again with food.
Tonight I had supper at a barbecue-type event. I took insulin inside the building and then went out to get my food. It turned out that I did not eat as much carb as I had planned and I ended up low afterward. This reminded me of an important message: it’s very – very – important never to take rapid-acting insulin before leaving home if you are eating out (at a restaurant or someone else’s house). Wait until you are seated, have ordered, and there is food in front of you. In other words, wait to take your mealtime insulin if you don’t know how long it will be or how much food you will eat. Better safe than sorry!